Weight-loss surgery is a drastic step.
In Linda Nelson's case, a surgeon removed 80 percent of her stomach, took out her gallbladder and disconnected, rearranged and reconnected her intestines.
TYPES OF BARIATRIC SURGERY
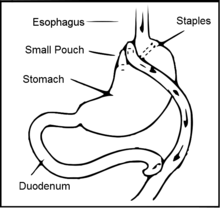
Roux-en-Y gastric bypass: This is the most common method of gastric bypass. It works by decreasing the amount of food a person can eat at one sitting and reducing absorption of nutrients. The surgeon cuts across the top of the stomach, sealing it off from the rest of the stomach. The resulting pouch is about the size of a walnut and can hold only about an ounce of food — down from the normal 3 pints. Then, the surgeon cuts the small intestine and sews part of it directly onto the pouch. Food then goes into this small pouch of stomach and then directly into the small intestine sewn to it.
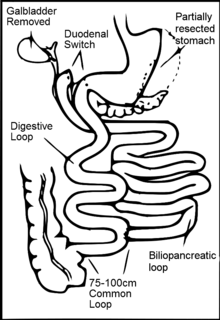
Biliopancreatic diversion with duodenal switch, or, simply, duodenal switch: About 80 percent of the stomach is removed. The valve that releases food to the small intestine remains, along with a limited portion of the small intestine (duodenum) that normally connects to the stomach. The surgery bypasses the majority of the intestine by connecting the end portion of the intestine to the duodenum near the stomach. This surgery limits how much a person can eat and reduces the absorption of nutrients. While it's very effective, it has more risks, including malnutrition and vitamin deficiencies. It's generally used for people who have a body mass index greater than 50.
Laparoscopic adjustable gastric banding: The surgeon positions an inflatable band around the uppermost part of the stomach. When the band is inflated, it compresses the stomach, acting like a tightening belt. This separates the stomach into two parts, with a very small upper pouch that communicates with the rest of the stomach through a channel created by the band. The small upper pouch limits the amount of food a person can eat. The band can be adjusted so that it restricts more or less food. Because of its relative simplicity, the operation is one of more common weight-loss surgeries. However, it may lead to less weight loss than may other procedures, and a person may need to have the band adjusted periodically.
Vertical banded gastroplasty: This procedure, also called stomach stapling, divides the stomach into two parts, restricting how much food a person can eat. The upper pouch is small and empties into the lower pouch — the rest of the stomach. Partly because it generally doesn't lead to adequate long-term weight loss, this weight-loss surgery isn't as popular as other types.
Sleeve gastrectomy: A sleeve gastrectomy, also called a vertical sleeve gastrectomy, is a newer type of weight-loss surgery. The sleeve gastrectomy actually is the first part of the surgical process for a biliopancreatic diversion with duodenal switch. However, the sleeve gastrectomy portion of surgery may be all that's needed to lose sufficient weight — in some cases the second part isn't needed. With sleeve gastrectomy, the structure of the stomach is changed to be shaped like a tube, which restricts the amount of calories a person's body absorbs.
Source: Mayo Clinic
The procedure already has worked wonders for her: She has lost 31 pounds since just before the Jan. 9 surgery. Five days after the surgery, she left Omaha's Methodist Hospital free of diabetes symptoms.
No more painful insulin shots. No more blood-sugar spikes that left her feeling shaky and jittery. No more diabetes medications.
Linda, who lives near Harlan, Iowa, is among a growing number of very overweight people undergoing the operations to not only lose weight but also rid themselves of the symptoms of Type 2 diabetes.
Not all who have the surgery become symptom-free, and for some that effect fades after a few years.
But for those whose diabetes symptoms go away, the effect usually is immediate — before any significant weight loss.
Researchers aren't sure why that is, but they're working to identify the process in an attempt to create drugs that could help with the treatment of diabetes.
Dr. John Anderson, the president of medicine and science for the American Diabetes Association, said the surgery is appropriate for severely obese people, particularly those who have shown an inability to lose weight. The evidence that it's right for moderately obese people, he said, is less compelling.
The surgery comes with risks and high costs, and not all insurance policies cover the procedure. In some cases, diabetes symptoms don't go away after surgery. When they do, some patients must resume taking diabetes medications after five years or so.
Over the years, Linda had tried diets, weight-loss programs and exercise, but the weight wouldn't stay off.
“It just was very frustrating to know that you're spending all that money and nothing's happening,” she said.
Linda, who is 65, is 5 feet tall. A couple of days before her surgery, she weighed 280 pounds. She has had Type 2 diabetes for four years. A little over a year ago, she developed a severe blood infection and was hospitalized for eight days. Her family physician wasn't sure that the diabetes was to blame, she said, but it certainly didn't help.
The doctor recommended that she consider weight-loss surgery.
Diabetes, both Types 1 and 2, is on the rise in the U.S.: From 1980 through 2010, the CDC says, the number of Americans with diagnosed diabetes more than tripled. The total number of people with diabetes, both diagnosed and undiagnosed, is more than 8 percent of the U.S. population.
People with diabetes can experience nerve, kidney, eye and blood-vessel damage. They face an increased risk of heart attacks and stroke.
The weight-loss surgeries allow many people with Type 2 diabetes, especially those not as severely affected, to go off all diabetes medications.
Medical experts don't know why people can stop taking their diabetes medicine so quickly after the surgeries, but they say hormones play a role.
In the operation Linda decided to have, a complicated one called a duodenal switch, the surgeon takes a patient's football-sized stomach down to bratwurst-size and reconnects the upper intestine so food from the stomach and digestive enzymes move through separate channels. They don't mix like they did before the surgery until they meet toward the end of the small intestine.
The intestinal reconfiguration also means that people don't absorb important nutrients, so they must take dietary supplements for the rest of their lives.
Linda's surgeon, Dr. Gary Anthone, said the duodenal switch works in a variety of ways: You eat less because your stomach is smaller; you absorb less because your intestine is shorter; you absorb less fat because bile and food don't have as much time to mix together; and you're presenting food to the lower part of your intestine more quickly. Moving the food lower in the intestine, it is thought, triggers the hormone that makes your pancreas secrete more insulin, and that tells your cells to respond to insulin better.
Steven Munger, a professor and researcher at the University of Maryland School of Medicine, said one theory is that the removal of tissue through these surgeries also removes some factor that promotes diabetes, or insulin resistance. Another, he said, echoing Anthone's explanation, is that in some weight-loss surgeries, part of the intestine is bypassed so that food goes from the stomach into a lower part of the intestine than it normally would, thus producing more “anti-diabetic” hormones.
Two other possibilities, Munger said: It's neither of those or it's some combination of the two.
Determining exactly what's happening, he said, could lead to the identification of a diabetes drug that would mimic the changes that occur in a person's physiology after the operation. “That would seem to be a nice way to go — to not have to go through this, which is a very significant surgery.”
From 2009 through 2011, 45,000 Medicare patients had weight-loss surgery. The American Society for Metabolic & Bariatric Surgery, a national group of weight-loss surgeons, estimates that 160,000 people in the U.S. had the operations in 2010. That's down from estimates for previous years of 200,000 surgeries annually, said Dr. Jaime Ponce, the society's president. Ponce attributed the drop, in part, to patients' out-of-pocket costs and insurance restrictions on coverage.
Although the totals are down, he and other surgeons said more people are turning to the surgeries to address diabetes.
Anderson, of the diabetes association, noted that while the surgeries are a good alternative for the right patients, they're still surgeries.
“The complication rates in the hands of experienced people is very low,” he said, “but it's not zero.”
Complications can include infections, leaks, internal hernias, ulcers, gallstones and blood clots. Since Linda had her surgery, she has vomited a few times when she tried to eat too large a portion, and has battled heartburn. Anthone, her surgeon, prescribed heartburn medication at her three-week check.
Anthone said he has performed 2,500 duodenal switch operations since 1992. It used to be, he said, that leaks — from the altered stomachs or the reconnected intestines — would occur in 5 to 10 percent of the cases. Today, he said, that rate is down to .5 percent to 1 percent of cases. “Locally, I would say we're even better than that,” he said.
How well the procedures combat Type 2 diabetes over the long term depends on how advanced someone's diabetes was when they had the surgery, according to a Seattle researcher.
Dr. David Arterburn, an associate investigator at the Group Health Research Institute in Seattle, said his recently published research found that people who have had diabetes for a long time, who already are on insulin or have poor control of their diabetes are much less likely to see their diabetes symptoms go away after gastric bypass surgery than are people with less-severe diabetes. Those with more-severe symptoms, he said, also were more likely to redevelop diabetes within five years.
“It didn't really matter what your weight change was,” he said.
Arterburn and other researchers looked at more than 4,400 people with diabetes who had a Roux-en-Y gastric bypass. More than 68 percent saw a complete remission of their diabetes symptoms. But of those, more than a third saw their symptoms return within five years.
Still, Arterburn said, people with diabetes who are severely obese should talk to their physicians about weight-loss surgery. Even if their diabetes symptoms don't go away, he said, the disease may be better controlled and they will move around better. And if they experience even just a short period of remission from their symptoms, he said, they will benefit.
Dr. Kalyana Nandipati, a surgeon and assistant professor at Creighton University School of Medicine, said some researchers have suggested that because of the surgeries' impact on diabetes symptoms, the operations should be performed on people who aren't morbidly obese. He also said the procedures could prevent diabetes from ever developing, citing a study, reported on last fall, that followed 3,400 obese men and women over 15 years. The Swedish researchers found that weight-loss surgery reduced the study participants' risk for developing Type 2 diabetes by 78 percent.
Linda Nelson was all smiles at a follow-up appointment almost three weeks after her bariatric surgery. After years of failed weight-loss efforts, she is optimistic this time: “I think it's a very doable thing,” she said. CHRIS MACHIAN/THE WORLD-HERALD
The surgeries “are not just to make people skinny but make them healthy,” Nandipati said.
Dr. Jennifer Larsen, a diabetes researcher and vice chancellor of research at the University of Nebraska Medical Center, argues that people with diabetes don't have to do something as drastic as undergoing surgery to lose some weight and gain better control over their disease.
“It is important for people to recognize there is an immediate cost and potential risk of surgery that usual care for diabetes doesn't have,” she said.
Ponce, from the national bariatric surgeons group, said certain types of weight-loss surgeries for severely obese patients who have other health problems are covered by some private insurers, as well as Medicare; Tricare, which is the insurance program for active and retired military and their dependents; and 47 state Medicaid programs. United Healthcare and Blue Cross Blue Shield of Nebraska say their standard policies don't cover such operations.
Linda's husband, Adrian, is glad that her insurance policy covers the procedure. When he opened the bill last week and saw that the charge for her surgery alone was more than $28,000, he grabbed his heart as if he were having a heart attack.
Dr. Cori McBride, a Nebraska Medical Center surgeon, said some insurers have told her that they don't want to pay for weight-loss surgeries because it takes several years to recoup the cost. Ponce said he had been told the same thing. The insurers, he said, say they won't see the benefit of what they spend because the average person changes insurance companies every two or three years.
Blue Cross Blue Shield of Nebraska provided a written statement acknowledging the procedures' costs. “We have excluded surgical treatment for morbid obesity as a standard contract term,” the statement reads, “to stay comparable with competitors and avoid passing on the costs to our customers.”
McBride noted that people who choose to have the operations must change their behaviors afterward. “They still have to watch things that they eat, eat healthy foods, modify their portions, eat when they're hungry, stop when they're full and not graze on garbage all day long.
“Unless they are committed to making the changes,” she said, “we shouldn't do the surgery.”
Anthone told Linda that she most likely will lose 60 to 80 percent of her excess body weight — between 96 and 129 pounds — within 18 months. Linda, who returned to work on Monday, said she's optimistic that will happen. “I do have the moral support, with Adrian, and I have my friends,” she said. “I think it's a very doable thing.”















.jpg)
.jpg)


.jpg)
.jpg)