Bariatric surgery includes a variety of procedures performed on people who are obese. Weight loss is achieved by reducing the size of the stomach with a gastric band or through removal of a portion of the stomach (sleeve gastrectomy or biliopancreatic diversion with duodenal switch) or by resecting and re-routing the small intestines to a small stomach pouch (gastric bypass surgery).
Long-term studies show the procedures cause significant long-term loss of weight, recovery from diabetes, improvement in cardiovascular risk factors, and a reduction in mortality of 23% from 40%. However, a study in Veterans Affairs (VA) patients has found no survival benefit associated with bariatric surgery among older, severely obese people when compared with usual care, at least out to seven years.
The American Society for Metabolic and Bariatric Surgery (ASMBS) is the largest society of healthcare professionals dedicated to the safe and effective provision of bariatric surgery. The vision of the Society is to improve public health and well being by lessening the burden of the disease of obesity and related diseases throughout the world. Founded in 1983, the purpose of the society is to advance the art and science of metabolic and bariatric surgery by continually improving the quality and safety of care and treatment of people with obesity and related diseases by:
The U.S. National Institutes of Health recommends bariatric surgery for obese people with a body mass index (BMI) of at least 40, and for people with BMI 35 and serious coexisting medical conditions such as diabetes. However, research is emerging that suggests bariatric surgery could be appropriate for those with a BMI of 35 to 40 with no comorbidities or a BMI of 30 to 35 with significant comorbidities.
From Wikipedia
Contents
Classification of
surgical procedures
Procedures
can be grouped in three main categories: Standard of care in the United
States and most of the industrialized world in 2009 is for laparoscopic as
opposed to open procedures. Future trends are attempting to achieve similar or
better results via endoscopic procedures.
Predominantly
malabsorptive procedures
In
predominantly malabsorptive procedures,
although they also reduce stomach size, the effectiveness of these procedures
are derived mainly from creating a physiological condition of malabsorption.

Diagram of a biliopancreatic diversion.
Biliopancreatic Diversion
This complex
operation is termed biliopancreatic diversion (BPD) or
the Scopinaro procedure. The original form of this procedure is now
rarely performed because of problems with malnourishment. It has been replaced
with a modification known as duodenal switch (BPD/DS). Part of
the stomach is resected, creating a smaller
stomach (however the patient can eat a free diet as there is no restrictive component).
The distal part
of the small intestine
is then connected to the pouch, bypassing the duodenum and jejunum.
In around 2% of
patients there is severe malabsorption and nutritional
deficiency that requires restoration of the normal absorption. The
malabsorptive effect of BPD is so potent that those who undergo the procedure
must take vitamin and dietary minerals above and beyond that
of the normal population. Without these supplements, there is risk of serious
deficiency diseases such as anemia and osteoporosis. Because gallstones are a common complication
of the rapid weight loss following any type of bariatric surgery, some surgeons
remove the gallbladder as a
preventive measure during BPD. Others prefer to
prescribe medications to reduce the risk of
post-operative gallstones. Far fewer surgeons perform BPD compared to other
weight loss surgeries, in part because of the need for long-term nutritional
follow-up and monitoring of BPD patients.
Jejunoileal bypass
This
procedure is no longer performed.
Endoluminal sleeve
A
study on humans was done in Chile using the same technique, however the
results were not conclusive and the device had issues with migration and
slipping. A study recently done in the Netherlands found a decrease of 5.5 BMI
points in 3 months with an endoluminal sleeve.
Predominantly
restrictive procedures
Procedures
that are solely restrictive, act to reduce oral intake by limiting gastric
volume, produces early satiety, and leave the alimentary canal in continuity,
minimizing the risks of metabolic complications.

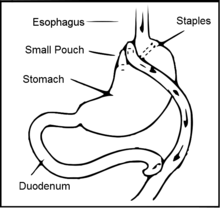
Diagram of a vertical banded gastroplasty.
Vertical Banded Gastroplasty
In the vertical
banded gastroplasty, also called the Mason procedure or stomach
stapling, a part of the stomach is permanently stapled to create a smaller
pre-stomach pouch, which serves as the new stomach.

Diagram of an adjustable gastric banding.
Adjustable gastric
band
The restriction
of the stomach also can be created using a silicone band, which can be adjusted
by addition or removal of saline through a port placed just under the skin.
This operation can be performed laparoscopically, and is commonly referred to
as a "lap band". Weight loss is
predominantly due to the restriction of nutrient intake that is created by the
small gastric pouch and the narrow outlet. It is considered one of the
safest procedures performed today with a mortality rate of 0.05%.
Sleeve gastrectomy
Sleeve
gastrectomy, or gastric sleeve, is a surgical weight-loss procedure in which
the stomach is reduced to about 15% of its
original size, by surgical removal of a large portion of the stomach, following
the major
curve. The open edges are then attached together (typically
with surgical staples,
sutures, or both) to leave the stomach shaped more like a tube, or a sleeve,
with a banana shape. The procedure permanently reduces the size of the stomach.
The procedure is performed laparoscopically and is not
reversible.
This combined
approach has tremendously decreased the risk of weight loss surgery for
specific groups of patients, even when the risk of the two surgeries is added.
Most patients can expect to lose 30 to 50% of their excess body weight over a
6–12 month period with the sleeve gastrectomy alone. The timing of the second
procedure will vary according to the degree of weight loss, typically 6 – 18
months.
·
Stomach volume is reduced, but it
tends to function normally so most food items can be consumed in small amounts.
·
Removes the portion of the stomach
that produces the hormones that stimulates hunger (Ghrelin), although the
durability of this removal has yet to be confirmed.
·
Dumping syndrome is less likely due to the preservation of
the pylorus (although dumping can occur anytime stomach surgery takes place).
·
Minimizes the chance of
an ulcer occurring.
·
By avoiding the
intestinal bypass, the chance of intestinal obstruction (blockage), anemia,
osteoporosis, protein deficiency and vitamin deficiency are significantly
reduced.
·
Very effective as a
first stage procedure for high BMI patients (BMI >55 kg/m2).
·
Limited results appear
promising as a single stage procedure for low BMI patients (BMI 35–45 kg/m2).
·
Appealing option for
people with existing anemia, Crohn's disease, irritable bowel syndrome, and
numerous other conditions that make them too high risk for intestinal bypass
procedures.
Intragastric Balloon
(gastric balloon)
Intragastric
balloon involves placing a deflated balloon into the stomach,
and then filling it to decrease the amount of gastric space. The balloon can be
left in the stomach for a maximum of 6 months and results in an average weight
loss of 5–9 BMI over half a year. While not yet approved by the FDA the
intragastric balloon is approved in Australia, Canada, and Mexico, India and
several European and South American countries. The intragastric balloon
may be used prior to another bariatric surgery in order to assist the patient
to reach a weight which is suitable for surgery, further it can also be used on
several occasions if necessary.
Gastric Plication
Basically, the
procedure can best be understood as a version of the more popular gastric sleeve or gastrectomy surgery where a sleeve is
created by suturing rather than removing stomach tissue thus preserving its
natural nutrient absorption capabilities. Gastric Plication significantly
reduces the volume of the patient's stomach, so smaller amounts of food provide
a feeling of satiety. The procedure is producing some significant results
that were published in a recent study in Bariatric Times and are based on
post-operative outcomes for 66 patients (44 female) who had the gastric sleeve
plication procedure between January 2007 and March 2010. Mean patient age was
34, with a mean BMI of 35. Follow-up visits for the assessment of safety and
weight loss were scheduled at regular intervals in the postoperative period. No
major complications were reported among the 66 patients. Weight loss outcomes
are comparable to gastric bypass.
The study
describes gastric sleeve plication (also referred to as gastric
imbrication or laparoscopic greater curvature plication)
as a restrictive technique that eliminates the complications associated with
adjustable gastric banding and
vertical sleeve gastrectomy—it
does this by creating restriction without the use of implants and without
gastric resection (cutting) and staples.
Mixed procedures
Mixed procedures apply
both techniques simultaneously.
Roux-en-Y gastric bypass.
Gastric bypass surgery
A common form
of gastric bypass
surgery is the Roux-en-Y gastric bypass. Here, a small stomach
pouch is created with a stapler device, and connected to the distal small
intestine. The upper part of the small intestine is then reattached in a
Y-shaped configuration. The gastric bypass had been the most commonly performed
operation for weight loss in the United States, and approximately 140,000
gastric bypass procedures were performed in 2005. Its market share has
decreased since then and by 2011, the frequency of gastric bypass was thought
to be less than 50% of the weight loss surgery market. A factor in the
success of any bariatric surgery is strict post-surgical adherence to a healthier
pattern of eating.
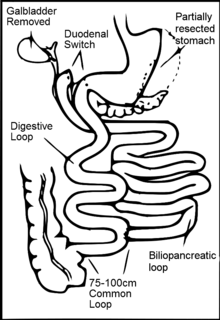
Diagram of a sleeve gastrectomy with duodenal
switch.
Sleeve Gastrectomy
with Duodenal Switch
A variation of
the biliopancreatic diversion includes a duodenal switch. The part of the stomach along its greater curve is
resected. The stomach is "tubulized" with a residual volume of about
150 ml. This volume reduction provides the food intake restriction component of
this operation. This type of gastric resection is anatomically and functionally
irreversible. The stomach is then disconnected from the duodenum and connected
to the distal part of the small intestine. The duodenum and the upper
part of the small intestine are reattached to the rest at about 75–100 cm
from the colon.
Implantable gastric
stimulation
This procedure
where a device similar to a heart pacemaker is implanted by a surgeon, with the
electrical leads stimulating the external surface of the stomach, is being
studied in the USA. Electrical stimulation is thought to modify the activity of
the enteric nervous
system of the stomach, which is interpreted by the brain to
give a sense of satiety, or fullness. Early evidence suggests that it is less
effective than other forms of bariatric surgery.












0 comments:
Post a Comment